New Press Fellows arrive at Wolfson

Retired Fellow Professor Gordon Dougan, a world authority on vaccines, genomics and the epidemiology of infectious diseases, argues that the developed world needs to remember the threat of epidemics.

Over the past 70 years we, living in the richer nations, have gradually lost our sense of danger concerning epidemics and serious infections. This is a consequence of better vaccines, improved health infrastructure and other medicines such as antibiotics that essentially drove serious community infections out of vision. This was not true everywhere in the world, where infections and epidemics continued to ravage the poorer regions. We in the richer world must now reacquire this instinctive memory post COVID-19.
Life in the modern world has changed dramatically over the last 70 years. Rapid global transport and communications interconnect and cocoon us all in a relatively ‘safe’ bubble. In the richer countries, until COVID-19, we were rarely troubled as a populous by infections outside of hospitals. Infections normally happened to others and we saw them only rarely at a personal level. There were and still are exceptions. Influenza remains common but is often mistaken for a severe cold or undiagnosed fever. We have outbreaks of infections in hospitals, such as C. difficile, which are dramatic and lethal but remain largely hidden from the community and mainly impact the old (1). Consequently, we have forgotten about the threat of epidemics. This has driven complacency, misunderstanding and an under appreciation of the things that preserve the bubble; vaccines, antibiotics, clean water and herd protection.
When I was a child in the 1950s, epidemics still occurred. We had regular outbreaks of measles (Figure 1), rubella and mumps, whilst skin boils (abscesses) and impetigo were still common in Northern England where I grew up. Typhoid outbreaks still occurred in the United Kingdom, such as in Aberdeen in 1964 (2) and the deadly disease smallpox still stalked the world (3). Polio was still crippling children and pneumonia was common (I was hospitalised with this as a young teenager). I also caught infectious jaundice (almost certainly Hepatitis A), which could not then be diagnosed, keeping me off school for weeks. GPs were freely available to visit the sick daily and hospital wards were run by dominant matrons imposing cleanliness and hygiene. Everyone was acutely aware of the infection threat.
As health systems were steadily built up over the next decades the immediate threat of infection gradually dissipated in richer countries, due to our increasing ability to control, diagnose and prevent infections. As a consequence – we have forgotten those days.
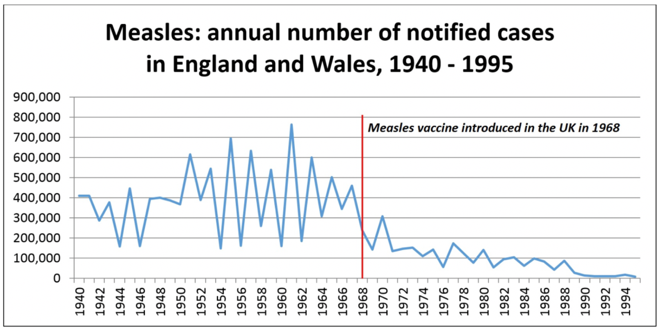
Source: Public Health England
Figure 1. Measles in the United Kingdom occurred regularly as periodic epidemics. The disease is now largely controlled by vaccination in the UK but it has not gone away
This is only half the story. Infections and epidemics still rage on in the poorer parts of the world. These are largely invisible to most of us in the richer areas, even though they kill millions of children each year. Malaria, dengue, worm infestations, measles and even diphtheria are still relatively common, particularly where there is social disruption (4). For example, 100,000’s of children have been struck by a raging cholera epidemic in Yemen in the past 3 years (Figure 2) (5, 6).
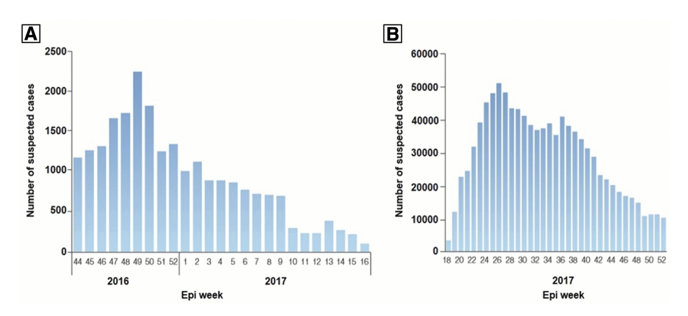
Figure 2. Trajectory of the recent cholera outbreak in Yemen (A) The first wave of the epidemic covering late 2016 through to early 2017 and (B) The second devastating huge wave of cholera in 2017. Taken from “Cholera situation in Yemen, December 2017,” and supplied by the World Health Organization. This figure also appears at www.ajtmh.org.
I regularly work and visit these settings to study epidemic cholera, antibiotic resistant typhoid and other diseases. In our work, we have uncovered hidden typhoid epidemics creeping across Asia and on into Africa (7). I have visited hospitals where the ward floor is crowded with children resting in their mother’s arms, infected with an antibiotic resistant salmonella with an untreated mortality of 50% (8). Hundreds of thousands of children have been lost – we know little of this in our richer world.
Now the threat has returned to us in the form of COVID-19 and we are not prepared. We are frightened and threatened by the invisible foe. Where is it? What is this coronavirus pathogen and what will it do to me or my loved ones? What should we do? Experts (and many, many non-experts) are willing to give us advice where there are few, if any, precedents of this type of infection rampaging in a population that lacks immunity. Where is the vaccine to protect us? Where now are those who have questioned the dangers of vaccination without balancing this against the benefits? Where is that frightening matron? Droplet dispersion is how diphtheria spreads. The bacteria that cause diphtheria is still present here in the richer world but we are protected through vaccination (4).
What is the value of experts like me? I likely know more about infection, epidemics and vaccines than most. I have studied epidemics across the world. I have made and designed vaccines. Do I know what will happen next with this epidemic? Which of the experts are right? The World Health Organisation (WHO)? The politicians and their teams of scientists and modellers?
In reality, we are all trying to take informed guesses. This is a new disease (or is it, has it been somewhere before, perhaps concealed locally in some region?). Do similar coronaviruses, such as those that cause common colds or even SARS protect us (9)? I support anyone trying to constructively intervene. The UK Government team are working with the best information, trying to predict the future. I back them, as I do the WHO.
Although COVID-19 is incredibly transmissible and infectious it is, fortunately, not currently a highly virulent virus. This does not soften the devastation felt by those close to people who lost their lives to it, but it is true overall. Additionally, if the virus gets into large vulnerable populations, which it could, that will also be tragic. However, we need to be continuously vigilant, as it could become more virulent as it further adapts to humans. It mostly causes serious disease predominantly in the unfortunate people who fall into the relatively few susceptible groups. With coronavirus it is mainly the older and the immuno-compromised who are vulnerable. We are lucky, in Africa Salmonella is killing 100,000s of children each year – thankfully, coronavirus looks so far to be largely sparing children. As most people who are infected with COVID-19 display few or relatively mild symptoms, it appears to have the hidden ‘advantage’ that it is likely providing some immunity, rather like a sort of nasty stealth vaccine. However, even here we know little about how protection works and how long it lasts.
In many ways we are lucky so far. This could have been a MUCH more aggressive and virulent virus. We need to deal with it as quickly as possible to make sure it does not mutate and change. Usually viruses become less virulent as an epidemic expands, but not always.
We need to try to limit the spread using our natural protective instincts. Limit contact, respect distance and think of others, particularly those who are most vulnerable.
Gordon Dougan is a Professor in the Department of Medicine, University of Cambridge and has spent his career leading research into vaccines, pathogen genomics and disease tracking. His research work has helped to redefine our understanding of how infections spread around the world, a subject of direct relevance to the current Covid-19 epidemic. These are his personal thoughts on the COVID-19 epidemic. Follow him on Twitter @GordonDougan1.
The author is supported by grants from Wellcome, NIMR, UKRI (Vaccine Hub), Gates Foundation. He would like to thank Sophie Palmer, Christine Hale, Kat Holt and Lara Marks for suggestions and edits. The author acknowledges and respects all those who have lost loved ones through infections.







